Cybersecurity challenges of healthcare inventory management are more than just a tech problem; they’re a potential patient safety crisis waiting to happen. Think about it: every needle, every bandage, every life-saving drug—all tracked digitally, all vulnerable to attack. From data breaches exposing sensitive patient information to compromised medical devices halting crucial treatments, the stakes are incredibly high. This exploration dives into the vulnerabilities, risks, and solutions needed to secure our healthcare supply chains.
We’ll unpack the real-world impact of data breaches, explore the unique vulnerabilities of connected medical devices, and delve into the often-overlooked threats of insider activity and compromised supply chains. We’ll also navigate the complex regulatory landscape and discuss practical strategies for securing physical inventory and managing third-party vendor risks. Get ready to upgrade your understanding of healthcare cybersecurity—because the future of patient care depends on it.
Data Breaches and Their Impact
Healthcare inventory management, while crucial for patient care, presents a significant cybersecurity vulnerability. The sensitive nature of the data involved – patient information, supplier details, financial transactions – makes it a prime target for malicious actors. Data breaches in this area can have far-reaching and devastating consequences, impacting not only the healthcare provider but also patients and the wider healthcare ecosystem.
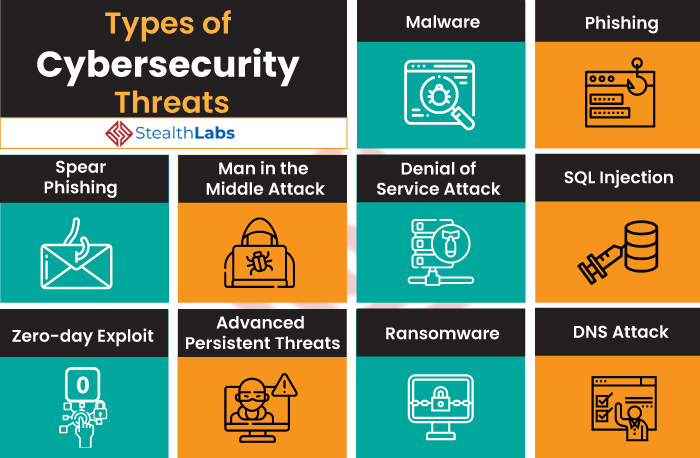
Types of Data Breaches in Healthcare Inventory Management
Data breaches in healthcare inventory management can take various forms. These range from simple unauthorized access to sophisticated attacks exploiting vulnerabilities in systems. A common type is the theft of credentials, allowing attackers to access sensitive data. Another is the exploitation of software vulnerabilities, such as unpatched systems or weak passwords, leading to unauthorized access or data exfiltration. Finally, insider threats, where employees or contractors misuse their access privileges, pose a significant risk. These breaches can expose a wide range of sensitive data, including patient medical records linked to specific inventory items, supplier contracts containing pricing and financial details, and internal communications detailing inventory management strategies.
Consequences of Data Breaches
The consequences of a data breach in healthcare inventory management can be severe and far-reaching. Financially, organizations face hefty fines and penalties under regulations like HIPAA in the US. Reputational damage can be equally crippling, leading to loss of patient trust and potential business decline. Legally, organizations can face lawsuits from affected patients and regulatory bodies, resulting in substantial legal fees and settlements. Beyond these direct costs, the breach can disrupt operations, leading to delays in patient care and increased administrative burdens. The long-term impact on patient trust and the organization’s ability to attract new patients or secure funding can be substantial.
Mitigating the Risk of Data Breaches
Implementing robust security measures is crucial to mitigate the risk of data breaches. This starts with strong access controls, including multi-factor authentication and regular password changes. Regular security audits and penetration testing identify and address vulnerabilities before they can be exploited. Employee training programs educate staff on cybersecurity best practices, including recognizing and reporting phishing attempts and other social engineering tactics. Keeping software up-to-date with security patches is essential, as is encrypting sensitive data both in transit and at rest. Finally, a comprehensive incident response plan ensures a swift and effective response in the event of a breach, minimizing its impact.
Examples of Real-World Healthcare Data Breaches
Several real-world examples highlight the devastating consequences of data breaches in healthcare. The following table illustrates some notable incidents:
| Date | Organization | Type of Breach | Impact |
|---|---|---|---|
| October 2022 (Example) | [Fictional Hospital Name] | Phishing attack leading to credential theft | Exposure of patient data linked to medical device inventory, resulting in HIPAA fines and reputational damage. |
| March 2023 (Example) | [Fictional Medical Supply Company] | Ransomware attack | Disruption of inventory management system, leading to delays in patient care and significant financial losses. |
| June 2024 (Example) | [Fictional Pharmacy] | Insider threat | Unauthorized access and theft of patient prescription data and inventory control information, leading to legal action and loss of trust. |
| September 2021 (Example) | [Fictional Health System] | Vulnerable software exploitation | Data breach affecting patient records tied to specific medical supplies, resulting in significant financial penalties and reputational harm. |
Vulnerabilities of Connected Medical Devices
The increasing reliance on connected medical devices in healthcare inventory management presents a significant cybersecurity challenge. These devices, ranging from insulin pumps to infusion systems and even simple monitoring equipment, often lack robust security features, creating vulnerabilities that can be exploited by malicious actors. This vulnerability extends beyond simple data breaches; it poses direct threats to patient safety and the integrity of the entire healthcare system.
The integration of these devices into inventory systems, while aiming for efficiency, introduces additional attack vectors. The interconnected nature of these systems means a breach in one device could potentially compromise the entire network, impacting not only inventory tracking but also patient care. Understanding these vulnerabilities and implementing robust security measures is paramount to mitigating these risks.
Insecure Communication Protocols
Many connected medical devices rely on outdated or insecure communication protocols, such as Telnet or FTP, which are easily susceptible to eavesdropping and manipulation. These protocols lack encryption and authentication, leaving sensitive data, including patient information and device configurations, exposed to unauthorized access. For instance, a hacker could intercept communication between a device and the inventory system, altering inventory counts or even remotely controlling the device itself. This could lead to medication shortages, inaccurate treatment plans, and potentially life-threatening situations. The use of modern, secure protocols like HTTPS and TLS is crucial to prevent such attacks.
Lack of Authentication and Authorization
Weak or nonexistent authentication mechanisms on connected medical devices allow unauthorized individuals to access and control them. This could involve simple password vulnerabilities or a complete lack of user authentication. A successful attack could lead to data theft, device manipulation, or even denial-of-service attacks, disrupting the entire inventory system and patient care. Implementing strong password policies, multi-factor authentication, and role-based access control are critical to mitigating this risk. For example, only authorized personnel should have access to change device settings or view sensitive patient data.
Software Vulnerabilities and Outdated Firmware
Many connected medical devices run on outdated operating systems and firmware, making them vulnerable to known exploits. Manufacturers often fail to provide timely security updates or patches, leaving devices exposed to cyberattacks. This is especially problematic because these devices often have long lifespans, meaning they remain vulnerable for extended periods. A real-world example is the discovery of vulnerabilities in insulin pumps that could allow attackers to remotely control insulin delivery. Regular software updates and firmware patching, along with robust vulnerability management processes, are essential for addressing this issue.
Insufficient Data Encryption
The transmission and storage of sensitive data related to inventory and patient care must be encrypted to prevent unauthorized access. However, many connected medical devices lack adequate encryption mechanisms, leaving data vulnerable during transmission and at rest. A data breach could expose patient medical records, device configurations, and other sensitive information, leading to significant privacy violations and legal repercussions. Employing strong encryption protocols, both in transit and at rest, is critical to safeguarding this information.
Secure Architecture for Integration
A secure architecture for integrating connected medical devices into the healthcare inventory management system should incorporate several key elements. This includes a dedicated, segmented network for medical devices, separate from the main hospital network, to limit the impact of a potential breach. Furthermore, robust firewalls and intrusion detection systems should be implemented to monitor network traffic and prevent unauthorized access. Regular security audits and penetration testing are crucial to identify and address vulnerabilities before they can be exploited. A well-defined security policy and comprehensive training program for healthcare staff are also essential to ensure that security best practices are followed.
Insider Threats and Access Control
Healthcare inventory management systems are treasure troves of sensitive data, making them prime targets for insider threats. These threats, originating from within the organization, can range from accidental data breaches to malicious intent, significantly impacting patient care and operational efficiency. Robust access control and proactive threat management are crucial to mitigating these risks.
Implementing effective security measures requires a multi-layered approach, combining technological safeguards with robust employee training and awareness programs. This approach needs to address the vulnerabilities inherent in human error and malicious intent, acknowledging that even well-intentioned employees can inadvertently compromise sensitive data.
Role-Based Access Control (RBAC) Implementation
Role-based access control (RBAC) is a cornerstone of secure inventory management. RBAC assigns permissions based on an individual’s job function, limiting access to only the data and systems necessary for their role. For instance, a nurse might have access to medication inventory but not financial records, while a procurement manager might have access to purchase orders and vendor information but not patient data. Implementing RBAC requires a careful analysis of job roles and responsibilities, followed by the creation of granular access profiles that reflect these roles. Regular audits of these profiles are essential to ensure that permissions remain appropriate and that no unnecessary access is granted. This prevents unauthorized access to sensitive data and minimizes the potential damage from insider threats.
Detecting and Responding to Suspicious Activity
Monitoring system logs for unusual activity is crucial for detecting potential insider threats. This includes tracking access attempts outside of normal working hours, unusual data access patterns, or attempts to modify system configurations. Sophisticated systems can leverage machine learning to identify anomalies and flag suspicious behavior for investigation. A well-defined incident response plan is critical for effectively handling suspected breaches. This plan should Artikel clear procedures for isolating compromised systems, containing the breach, investigating the cause, and remediating the vulnerability. Regular security audits and penetration testing can also help identify vulnerabilities before they can be exploited.
Best Practices for Employee Training and Awareness Programs
A comprehensive employee training program is vital in preventing insider threats. The program should cover the following:
- Data Security Policies: Employees must understand and adhere to the organization’s data security policies, including password management, access control procedures, and acceptable use of technology.
- Social Engineering Awareness: Training should educate employees on recognizing and avoiding social engineering tactics, such as phishing emails or pretexting attempts to gain access to sensitive information.
- Phishing Simulations: Regular phishing simulations can help assess employee awareness and reinforce training on identifying malicious emails and links.
- Reporting Procedures: Employees should be trained on how to report suspicious activity, ensuring they feel comfortable reporting incidents without fear of retribution.
- Data Handling Best Practices: Training should cover proper data handling procedures, including secure storage, transmission, and disposal of sensitive information.
- Regular Updates: Training should be regularly updated to reflect changes in technology and evolving threats.
Supply Chain Risks and Vulnerabilities
Healthcare inventory management faces significant cybersecurity challenges extending far beyond the hospital walls. The intricate web of suppliers, distributors, and storage facilities that constitute the healthcare supply chain presents a vast attack surface, ripe for exploitation by malicious actors. Compromising any link in this chain can lead to devastating consequences, from disruptions in patient care to the theft of sensitive data.
The healthcare supply chain’s vulnerability stems from its inherent complexity and the diverse range of actors involved. Each step, from the manufacturing of medical devices to their delivery to the point of care, introduces new potential weaknesses. This interconnectedness means a breach at one point can cascade through the entire system, impacting numerous stakeholders and creating widespread disruption. Understanding these vulnerabilities is crucial for implementing effective security measures.
Vulnerabilities in Procurement
The procurement process, often involving multiple vendors and complex contracts, is a prime target for cyberattacks. Phishing scams targeting procurement staff can lead to the compromise of sensitive financial information or the introduction of malicious software into the organization’s systems. Furthermore, counterfeit medical devices entering the supply chain pose a significant threat to patient safety and operational integrity. Robust verification processes, including secure communication channels and rigorous vendor vetting, are essential to mitigate these risks. For example, implementing multi-factor authentication for all procurement personnel and using blockchain technology to track the provenance of medical devices can significantly improve security.
Vulnerabilities in Distribution
The distribution phase, involving transportation and warehousing of medical supplies, introduces further vulnerabilities. Unsecured transportation vehicles can be targeted for theft or data breaches. Warehouse security lapses, such as inadequate access control or lack of surveillance, can allow unauthorized access to sensitive inventory or data. Real-time tracking systems using GPS and IoT sensors, coupled with robust physical security measures like access control systems and video surveillance, can help mitigate these risks. A case in point is the implementation of tamper-evident seals on packages and real-time tracking of shipments to deter theft and unauthorized access.
Vulnerabilities in Storage
Once medical supplies reach their destination, secure storage is paramount. Improper storage conditions can compromise the efficacy of medical devices, while inadequate security measures can lead to theft or damage. Environmental monitoring systems, coupled with robust access control and inventory management systems, are crucial for ensuring the integrity and security of stored supplies. For instance, using smart storage solutions with integrated security features, such as biometric access control and temperature sensors, can significantly reduce the risk of loss or compromise. Furthermore, regular audits of storage facilities and inventory are essential to identify and address any security weaknesses.
Implementing Supply Chain Security Measures, Cybersecurity challenges of healthcare inventory management
A comprehensive approach to securing the healthcare supply chain requires a multi-layered strategy involving collaboration across all stakeholders. This includes implementing robust cybersecurity protocols at each stage of the process, from procurement to storage. Regular security assessments, vulnerability scanning, and penetration testing are crucial for identifying and addressing potential weaknesses. Furthermore, employee training programs focusing on cybersecurity awareness and best practices are essential to prevent human error from becoming a point of failure. Regular updates of security software and hardware are also paramount.
Comparing Different Approaches to Securing the Healthcare Supply Chain
Different approaches to securing the healthcare supply chain exist, ranging from basic security measures to sophisticated, technology-driven solutions. A purely reactive approach, focusing solely on incident response, is insufficient to address the complex and evolving nature of supply chain threats. A proactive approach, involving risk assessment, vulnerability management, and preventative measures, is essential. Comparing these approaches highlights the need for a holistic strategy that integrates technological solutions with robust operational processes and strong collaboration among all stakeholders. For example, a company may choose to invest in blockchain technology for enhanced supply chain transparency, while another may prioritize strengthening physical security measures in their warehouses. The optimal approach depends on the specific context, resources, and risk profile of each organization.
Regulatory Compliance and Standards

Source: eos-intelligence.com
Navigating the complex world of healthcare inventory management requires a keen understanding of the regulatory landscape. Non-compliance can lead to hefty fines, reputational damage, and, most importantly, compromise patient safety. This section Artikels key regulations and best practices for ensuring your healthcare organization’s inventory management system is secure and compliant.
Maintaining regulatory compliance isn’t just about avoiding penalties; it’s about building a robust security framework that protects sensitive patient data and ensures the integrity of medical supplies. This involves a multi-faceted approach encompassing policy, procedures, technology, and ongoing monitoring.
Relevant Regulatory Standards and Compliance Requirements
The healthcare industry faces a multitude of regulations designed to protect patient data and ensure the safety and efficacy of medical devices and supplies. Adherence to these standards is crucial for any organization managing healthcare inventory.
A comprehensive compliance program needs to address several key areas. Understanding the specifics of each regulation and how they apply to inventory management is paramount.
- HIPAA (Health Insurance Portability and Accountability Act): This US law mandates the protection of Protected Health Information (PHI). Inventory systems storing patient data, even indirectly, must comply with HIPAA’s security and privacy rules. This includes data encryption, access controls, and audit trails.
- NIST Cybersecurity Framework (CSF): While not a law, the NIST CSF provides a voluntary framework for managing cybersecurity risk. Its five functions (Identify, Protect, Detect, Respond, Recover) offer a structured approach to building a secure inventory management system. Healthcare organizations often adapt the NIST CSF to meet their specific needs and HIPAA requirements.
- FDA (Food and Drug Administration) Regulations: The FDA regulates medical devices and their associated software. Inventory management systems that track medical devices must comply with relevant FDA regulations concerning device traceability, recall management, and data integrity. These regulations are particularly important for ensuring the safety and efficacy of medical devices.
- GDPR (General Data Protection Regulation): For organizations operating within the European Union or handling data from EU citizens, GDPR applies. Similar to HIPAA, GDPR focuses on the protection of personal data, requiring stringent data security measures within the inventory management system.
Achieving and Maintaining Compliance
Compliance is an ongoing process, not a one-time event. It requires a combination of proactive measures and continuous monitoring.
A multi-pronged approach is necessary to effectively achieve and maintain regulatory compliance. This involves establishing clear policies, implementing robust security controls, and conducting regular audits.
- Risk Assessment: Conduct a thorough risk assessment to identify vulnerabilities in your inventory management system and prioritize mitigation efforts.
- Policy Development and Implementation: Create and implement comprehensive policies addressing data security, access control, and incident response related to inventory management.
- Security Controls: Implement robust security controls, such as access control lists, data encryption, and regular security updates to software and hardware.
- Regular Audits and Monitoring: Conduct regular audits and security monitoring to ensure compliance with regulations and identify potential vulnerabilities.
- Employee Training: Provide regular training to employees on cybersecurity best practices and their responsibilities in maintaining compliance.
- Incident Response Plan: Develop and regularly test an incident response plan to address data breaches and other security incidents.
Integrating Compliance Requirements into the Inventory Management System
Compliance requirements should be woven into the fabric of the inventory management system, not treated as an afterthought.
Integrating compliance requirements into the system ensures that security is built-in from the ground up, rather than bolted on as an afterthought. This results in a more secure and efficient system.
- Access Control Integration: Integrate access control mechanisms to restrict access to sensitive inventory data based on roles and responsibilities.
- Audit Trails: Implement robust audit trails to track all access and modifications to inventory data, facilitating investigations and demonstrating compliance.
- Data Encryption: Encrypt sensitive data both in transit and at rest to protect it from unauthorized access.
- System Security Updates: Implement a system for regularly updating the inventory management system’s software and hardware to patch security vulnerabilities.
Best Practices for Documenting Compliance Efforts
Meticulous documentation is crucial for demonstrating compliance to auditors and regulators.
Comprehensive documentation not only aids in demonstrating compliance but also provides valuable insights for continuous improvement of security practices. It’s a vital part of proactive risk management.
- Risk Assessment Reports: Maintain detailed records of risk assessments, including identified vulnerabilities and mitigation strategies.
- Security Policies and Procedures: Document all security policies and procedures related to inventory management.
- Audit Logs: Regularly review and maintain audit logs of all system activities.
- Incident Response Records: Document all security incidents, including the response taken and lessons learned.
- Training Records: Maintain records of all employee training on cybersecurity best practices.
Physical Security of Inventory
Source: stealthlabs.com
Protecting healthcare inventory isn’t just about preventing financial losses; it’s about ensuring patient safety and maintaining operational efficiency. A compromised inventory can lead to delays in treatment, shortages of essential supplies, and even compromise the integrity of medical devices. Robust physical security measures are crucial for mitigating these risks.
Physical security measures safeguard healthcare inventory from theft, damage, and unauthorized access. These measures create a layered defense, combining environmental controls, access restrictions, and technological solutions to protect valuable assets and sensitive information associated with the inventory. Effective implementation relies on a holistic approach, encompassing careful planning, regular monitoring, and proactive risk mitigation strategies.
Securing Storage Areas
Secure storage areas are the cornerstone of effective inventory protection. This involves choosing appropriately sized, well-lit, and climate-controlled spaces. The location itself should be strategically chosen, minimizing external access points and maximizing visibility. Strong, reinforced doors and windows with tamper-evident seals are essential. Shelving should be organized to maximize space and visibility, preventing items from being easily hidden or misplaced. Regular inspections should be conducted to identify and address any potential vulnerabilities. For example, a hospital might use a dedicated, alarmed storage room with limited access points for high-value pharmaceuticals, while less sensitive supplies might be stored in a locked, well-lit cabinet.
Preventing Theft and Managing Access
Preventing theft requires a multi-pronged approach. This includes implementing strict access control protocols, utilizing surveillance systems, and regularly auditing inventory levels. Access should be limited to authorized personnel only, with individual accountability for inventory movements tracked through a robust system, such as barcoding or RFID tracking. Surveillance systems, including CCTV cameras and motion detectors, provide real-time monitoring and act as a significant deterrent. Regular inventory audits help to identify discrepancies and potential theft early on. For instance, a clinic might use a system where each nurse signs for medications they take from a locked cabinet, with regular stock checks conducted by a supervisor.
Utilizing Technology to Enhance Physical Security
Technology significantly enhances physical security measures. Access control systems, using key cards, biometric scanners, or PIN codes, restrict entry to authorized personnel only. Surveillance systems, incorporating high-resolution cameras and advanced analytics, provide real-time monitoring and recording capabilities, allowing for quick identification of suspicious activity. RFID (Radio-Frequency Identification) tags can be attached to individual items, enabling real-time tracking and preventing unauthorized removal. Integrated systems can combine access control, surveillance, and inventory management software to provide a comprehensive security solution. For example, a large hospital might use a centralized security management system that integrates CCTV footage, access logs, and inventory data to provide a holistic view of security and identify potential threats.
Example of a Secure Inventory Storage Facility
Imagine a dedicated warehouse for medical supplies. The building is equipped with a robust security fence, topped with barbed wire and monitored by motion detectors. Entry is controlled by a secured gate with a biometric scanner and 24/7 surveillance. Inside, multiple climate-controlled rooms are allocated for different inventory categories. Each room has reinforced doors with electronic locks, access granted only via a secured access control system. High-resolution CCTV cameras with night vision capabilities are strategically positioned throughout the facility, with recordings stored securely offsite. Shelving is organized logically, allowing for easy inventory checks. Regular patrols by security personnel supplement the electronic security systems. The entire facility is protected by a sophisticated alarm system connected to a central monitoring station.
Third-Party Vendor Risk Management: Cybersecurity Challenges Of Healthcare Inventory Management
Source: ttgtmedia.com
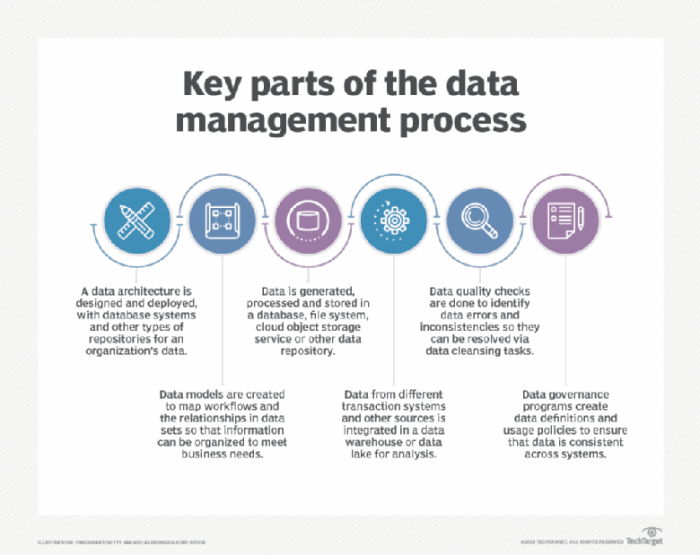
Healthcare inventory management often relies on third-party vendors for various services, from software solutions to data storage and transportation logistics. This reliance introduces significant cybersecurity risks, as vulnerabilities within a vendor’s systems can directly impact a healthcare organization’s sensitive patient data and operational integrity. Effective management of these risks is crucial for maintaining patient confidentiality, ensuring operational continuity, and complying with stringent healthcare regulations.
Third-party vendors introduce several layers of complexity to a healthcare organization’s security posture. Their own security practices, employee training, and physical security measures all become critical factors affecting the overall security of the healthcare provider’s inventory management system. A single breach within a vendor’s infrastructure can cascade through the entire supply chain, leading to devastating consequences.
Risks Associated with Third-Party Vendors
The use of third-party vendors in healthcare inventory management presents a range of cybersecurity risks. These risks extend beyond simple data breaches and encompass disruptions to operations, financial losses, and reputational damage. For example, a compromised vendor managing delivery routes could lead to the theft of valuable medical supplies or the exposure of patient data during transit. Similarly, a vendor providing software for inventory tracking might have vulnerabilities that allow unauthorized access to sensitive inventory details or patient information linked to those inventories. These risks necessitate a robust risk assessment and mitigation strategy.
Assessing and Mitigating Cybersecurity Risks
A comprehensive risk assessment should evaluate the vendor’s security controls, including their physical security measures, data encryption practices, access control policies, incident response plans, and employee training programs. This assessment should be thorough and go beyond simple questionnaires, potentially involving on-site inspections and penetration testing of the vendor’s systems. Mitigation strategies should address identified vulnerabilities, perhaps through the implementation of security controls within the healthcare organization’s systems or through collaborative efforts with the vendor to strengthen their security posture. Regular security audits and vulnerability scans are crucial for ongoing risk mitigation.
Importance of Contracts and Service Level Agreements (SLAs)
Contracts and SLAs are essential tools for addressing security concerns with third-party vendors. These legal agreements should clearly Artikel the vendor’s security responsibilities, including data protection measures, incident response procedures, and compliance with relevant regulations such as HIPAA. SLAs should define service availability, performance metrics, and penalties for security breaches. Furthermore, the contracts should specify the vendor’s liability in case of a data breach or other security incident, protecting the healthcare organization from potential financial and reputational damage. Regular review and updates of these contracts are vital to ensure they remain relevant and effective.
Framework for Managing Third-Party Vendor Risks
A robust framework for managing third-party vendor risks should incorporate the following key elements:
- Vendor Selection and Due Diligence: A rigorous selection process involving thorough background checks, security assessments, and reference checks.
- Risk Assessment and Mitigation: Regular assessments of the vendor’s security posture and implementation of appropriate mitigation strategies.
- Contractual Agreements: Comprehensive contracts and SLAs that clearly define security responsibilities and liabilities.
- Monitoring and Auditing: Continuous monitoring of the vendor’s performance and regular security audits.
- Incident Response Planning: A collaborative incident response plan that Artikels procedures in case of a security breach.
- Ongoing Communication and Collaboration: Open communication and collaboration between the healthcare organization and the vendor to address security concerns proactively.
This framework provides a structured approach to managing the inherent risks associated with using third-party vendors in healthcare inventory management, helping to protect sensitive patient data and ensure operational continuity.
Last Word
Securing healthcare inventory management isn’t just about protecting data; it’s about protecting lives. The interconnectedness of our healthcare systems means a single vulnerability can cascade into widespread disruption and devastating consequences. By understanding the diverse threats—from data breaches and insider threats to supply chain vulnerabilities and compromised devices—and implementing robust security measures, we can build a more resilient and secure healthcare ecosystem. The journey towards a truly secure healthcare inventory management system requires a multi-faceted approach, encompassing technological advancements, stringent regulatory compliance, and a culture of cybersecurity awareness. Let’s make patient safety the ultimate priority.